Surgery

Surgery Options for Obstructive Sleep Apnoea
For those who are unable to tolerate continuous positive airway pressure (CPAP) to treat their obstructive sleep apnoea (OSA), Several surgical procedure options are available to increase the size of the airway. However, they may be of limited effectiveness and it is difficult to predict which patients will do well with this procedure.
Some of the more common procedures include removal of adenoids, tonsils, nasal polyps or other growths and other tissue in the airway. Surgery is sometimes recommended, usually by ear, nose, and throat specialists, for severe obstructive sleep apnoea. A patient should be sure to seek a second opinion from a specialist in sleep disorders before proceeding with surgery.
Uvulopalatopharyngoplasty (UPPP)
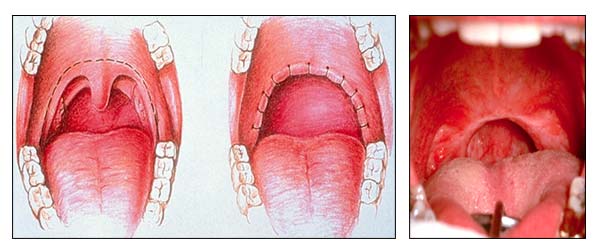
This is the most common surgical treatment in individuals with mild and moderate OSA who cannot tolerate CPAP or other medical management. UPPP is the surgical removal of excess tissue in the upper airway, including the back of the mouth and the throat.
UPPP involves the removal of tissue from the tonsils, uvula, and the hard palate (the roof of the mouth). These tissues may be obstructing the airway, and it is hoped that removing them will clear this obstruction.
There are various complications that can occur with the procedure. As with any surgical procedure, there are risks of pain, bleeding, and infection. In addition, there may be changes in the voice, a narrowing of the pharynx (called stenosis), a sensation of a foreign body in the throat, or the risk of velopharyngeal insufficiency (regurgitation of food, liquids, or saliva into the nose when swallowing). There may also be difficulties tolerating CPAP if it is needed after the procedure.
Only 50% of adults treated with UPPP cut their number of apnoea and hypopnoea events by half or more. These improvements may also diminish over time. It is considered a second-line therapy, after CPAP treatment, and only for those who have tissue obstruction of their airway.
Tracheostomy
Tracheostomy is a surgical incision in the front of the windpipe (trachea), with placement of a plastic tube to keep this open, and it is highly effective in treating OSA. It bypasses the obstruction of the upper airway, which is the primary cause of the disorder.
Due to its rather invasive nature, and the effectiveness of CPAP, it is rarely used. It is generally reserved for those with life-threatening disorders such as cor pulmonale, arrhythmias, or severe hypoxaemia (low blood oxygen levels) that cannot be controlled with other treatment.
Are There Other Surgical Options?
Depending on the cause of the apnoea, other surgical procedures may be appropriate to correct facial abnormalities or obstructions. They may be used alone or combined with each other or with UPPP. Most are invasive and reserved for patients with severe sleep apnoea who fail to respond to or comply with CPAP. They include:
- Genioglossus (tongue advancement), in which an opening is cut where the tongue joins the jawbone and the area is pulled forward.
- Temperature controlled radiofrequency ablation tongue reduction.
- Genioplasty, which is plastic surgery on the chin.
- Hyoid advancement surgery, in which the movable bone underneath the chin is moved forward, pulling the tongue muscle along with it.
- Maxillary or maxillomandibular advancement (MMA), which moves the upper (maxilla) or lower (mandible) jawbone forward. A survey of patients who had MMA found that the surgery changed their facial appearance, but most people thought it was a change for the better.
- Surgery for nasal obstructions (such as a deviated septum) that contribute to snoring and other symptoms.